Tarihin shiga tsakiyar venous
1. 1929: Likitan fiɗa na Jamus Werner Forssmann ya sanya wani ƙwayar fitsari daga gefen hagu na hagu na hagu, kuma ya tabbatar da X-ray cewa catheter ya shiga dama ta atrium.
2. 1950: An samar da catheters na tsakiya a matsayin sabon zaɓi don shiga tsakiya.
3. 1952: Aubaniac ya ba da shawarar huda jijiyoyin jini, Wilson daga baya ya ba da shawarar catheterization na CVC dangane da jijiyoyin subclavian.
4. 1953: Sven-Ivar Seldinger ya ba da shawarar maye gurbin allura mai wuya tare da jagorar jagorar waya mai jagora don venipuncture na gefe, kuma dabarar Seldinger ta zama fasahar juyin juya hali don sanyawa ta tsakiya venous catheter jeri.
5. 1956: Forssmann, Cournand, Richards sun sami lambar yabo ta Nobel a fannin likitanci saboda gudummawar da suka bayar ga catheterization na zuciya.
6. 1968: Rahoto na farko a cikin Ingilishi na samun damar shiga cikin jugular venous don saka idanu kan matsa lamba ta tsakiya
7. 1970: An fara gabatar da ra'ayin catheter tunnel
8. 1978: Venous Doppler Locator don na ciki jugular jijiya surface alama
9. 1982: Yin amfani da duban dan tayi don jagorantar hanyar shiga ta tsakiya ta Peters et al.
10. 1987: Wernecke et al na farko sun ba da rahoton yin amfani da duban dan tayi don gano pneumothorax
11. 2001: The Bureau of Health Research and Quality Evidence Reporting lists Central Venous access point-of-care duban dan tayi a matsayin daya daga cikin 11 ayyuka da suka cancanci tartsatsi gabatarwa.
12. 2008: American College of Emergency Physicians lists ultrasonic-guided Central venous access as a "core or primary gaggawa duban dan tayi"
13.2017: Amir et al sun ba da shawarar cewa za a iya amfani da duban dan tayi don tabbatar da wurin CVC kuma cire pneumothorax don adana lokaci da tabbatar da daidaito.
Ma'anar shiga ta tsakiya ta venous
1. CVC gabaɗaya yana nufin shigar da catheter a cikin tsakiyar jijiya ta cikin jijiya jugular na ciki, jijiya subclavian da jijiya na mata, yawanci tip na catheter yana cikin babban vena cava, ƙananan vena cava, caval-atrial junction, Dama atrium ko brachiocephalic vein, daga cikinsu akwai mafi girma vena cava.Venous ko rami-atrial junction an fi so
2. A gefe guda da aka saka catheter na tsakiya shine PICC
3. Ana amfani da damar shiga ta tsakiya musamman don:
a) Ƙarfafa allura na vasopressin, inositol, da dai sauransu.
b) Manyan catheters don jiko ruwan raɗaɗi da samfuran jini
c) Babban catheter don maganin maye gurbin koda ko maganin musanya na plasma
d) Gudanar da abinci mai gina jiki na iyaye
e) Maganin maganin rigakafi ko chemotherapy na dogon lokaci
f) Katar mai sanyaya
g) Sheaths ko catheters don wasu layukan, irin su catheters na huhu na huhu, wayoyi masu motsi da hanyoyin endovascular ko hanyoyin shiga tsakani na zuciya, da sauransu.
Ka'idodin asali na duban dan tayi jagorar CVC jeri
1.Assumptions na gargajiya CVC cannulation dangane da anatomical alamomi: sa ran jijiyoyin bugun gini anatomy da patency na veins
2. Ka'idodin Jagorar Ultrasound
a) Bambance-bambancen dabi'a: wurin jijiya, alamun jikin jiki da kansu;duban dan tayi damar real-lokaci gani da kima na tasoshin da m jikin mutum
b) Ƙunƙarar jini: Ultrasonography na farko zai iya gano thrombosis da stenosis a cikin lokaci (musamman a cikin marasa lafiya marasa lafiya tare da babban abin da ya faru na thrombosis mai zurfi)
c) Tabbatar da jijiyar da aka saka da kuma matsayi na catheter: lura da ainihin lokacin shigarwar guidewire cikin jijiya, brachiocephalic vein, ƙananan vena cava, dama atrium ko mafi girma vena cava.
d) Rage rikitarwa: thrombosis, tamponade na zuciya, huda jijiya, hemothorax, pneumothorax.
Zaɓin Bincike da Kayan aiki
1. Siffofin kayan aiki: Hoton 2D shine tushen, launi Doppler da pulsed Doppler na iya bambanta tsakanin arteries da veins, sarrafa rikodin likita a matsayin wani ɓangare na bayanan likita na marasa lafiya, murfin bincike mara kyau / coupplant yana tabbatar da warewa mara kyau.
2. Zabin bincike:
a) Shiga ciki: Jijiya na ciki da na mata yawanci suna da zurfin 1-4 cm a ƙarƙashin fata, kuma jijiyoyin subclavian suna buƙatar 4-7 cm.
b) ƙuduri mai dacewa da daidaitacce mayar da hankali
c) Ƙananan girman bincike: 2 ~ 4cm fadi, mai sauƙi don lura da tsayi da gajeren gatari na jini, sauƙi don sanya bincike da allura.
d) 7 ~ 12MHz ƙananan jeri na linzamin kwamfuta ana amfani da su gabaɗaya;ƙaramin convex a ƙarƙashin clavicle, binciken sandar hockey na yara
Hanyar gajeriyar axis da kuma hanyar dogon-axis
Dangantakar da ke tsakanin binciken da allura ta ƙayyade ko yana cikin jirgin sama ko kuma daga cikin jirgin
1. Ba za a iya ganin tip ɗin allura yayin aiki ba, kuma ana buƙatar ƙaddara matsayin titin allura ta hanyar jujjuya binciken;abũbuwan amfãni: gajeren koyo kwana, mafi kyau lura da perivascular nama, da kuma sauki jeri na bincike ga masu kitse da gajerun wuyansa;
2. Ana iya ganin cikakken jikin allura da titin allura yayin aikin;yana da ƙalubale don kiyaye tasoshin jini da allura a cikin jirgin hoton duban dan tayi a kowane lokaci
a tsaye da tsauri
1. A tsaye Hanyar, duban dan tayi ne kawai amfani da preoperative kima da zabi na allura maki
2. Dynamic Hanyar: ainihin-lokaci duban dan tayi-shiryar huda
3. Hanyar yin alama ta jiki <tsayayyen hanya <hanyar tsauri
Ultrasound-shiryarwar CVC huda da catheterization
1. Shirye-shiryen riga-kafi
a) Rijistar bayanan mara lafiya don adana bayanan ginshiƙi
b) Bincika wurin da za a huda don tabbatar da jiyya na jijiyoyin jini da patency, da ƙayyade tsarin tiyata.
c) Daidaita ribar hoto, zurfin, da sauransu don samun mafi kyawun yanayin hoto
d) Sanya kayan aikin duban dan tayi don tabbatar da cewa wurin huda, bincike, allo da layin gani suna collinear.
2. Intraoperative basira
a) Ana amfani da gishiri na Physiological a saman fata maimakon coupplant don hana couplant shiga jikin mutum.
b) Hannun da ba rinjaye ba yana riƙe binciken a hankali kuma ya jingina da sauƙi ga majiyyaci don daidaitawa.
c) Ka ɗora idanunka akan allon duban dan tayi, kuma ka ji canje-canjen matsin lamba da allura ta aika da hannunka (jin gazawar)
d) Gabatar da waya mai jagora: Marubucin ya ba da shawarar cewa a sanya aƙalla 5 cm na waya mai jagora a cikin jirgin ruwa na tsakiya (watau, waya jagora ya kamata ya kasance aƙalla 15 cm daga wurin allura);Bukatar shigar da 20 ~ 30cm, amma waya mai jagora ya shiga zurfi sosai, yana da sauƙi don haifar da arrhythmia.
e) Tabbatar da matsayin waya mai jagora: Yi nazari tare da gajeriyar axis sannan kuma tsayin daka na tashar jini daga nesa mai nisa, da kuma bibiyar matsayin wayar jagora.Misali, lokacin da aka huda jijiyar jugular na ciki, ya zama dole a tabbatar da cewa wayar jagora ta shiga cikin jijiyar brachiocephalic.
f) A yi ɗan guntuwar ƙanƙara kafin a tsaga, dilatar ta ratsa dukkan nassoshin da ke gaban magudanar jini, amma a guji huda magudanar jini.
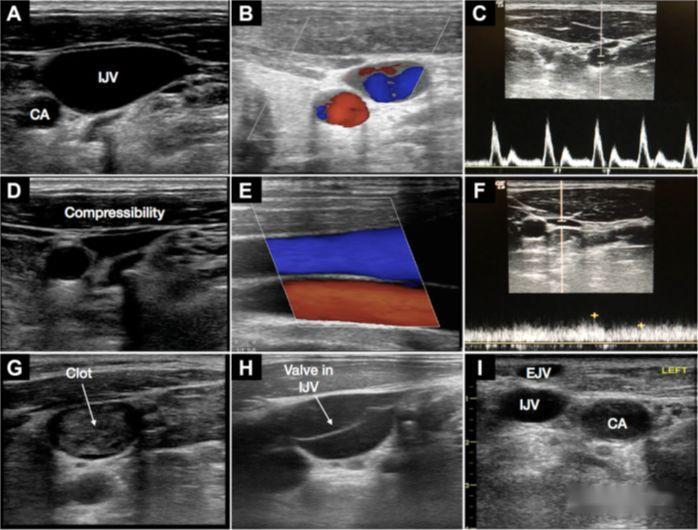
3. Tarkon Cannulation na Jugular Vein na ciki
a) Dangantakar da ke tsakanin jijiya carotid da jijiya na ciki: A zahiri, jijiya jugular na ciki gabaɗaya tana wajen waje na jijiya.A lokacin binciken gajeriyar axis, saboda wuyansa zagaye ne, dubawa a wurare daban-daban yana samar da kusurwoyi daban-daban, kuma veins da arteries na iya faruwa.Al'amari.
b) Zaɓin wurin shigar da allura: diamita na kusa yana da girma, amma yana kusa da huhu, kuma hadarin pneumothorax yana da girma;ana bada shawara don dubawa don tabbatar da cewa jinin jini a wurin shigarwar allura yana da zurfin 1 ~ 2cm daga fata
c) Bincika gaba dayan jijiya jugular na ciki a gaba, tantance yanayin jiki da patency na jini, guje wa thrombus da stenosis a wurin huda kuma raba shi da jijiyoyin carotid.
d) Guji huda bugun jini na carotid: Kafin vasodilation, wurin huda da matsayi na waya mai jagora yana buƙatar tabbatarwa a cikin dogon ra'ayi na axis.Don dalilai na aminci, dogon hoton axis na waya mai jagora yana buƙatar gani a cikin jijiya ta brachiocephalic.
e) Juya kai: Hanyar huda alamar gargajiya ta ba da shawarar juya kai don haskaka alamar tsokar sternocleidomastoid da fallasa da gyara jijiya jugular na ciki, amma juya kan digiri 30 na iya haifar da jijiyoyin jugular na ciki da artery carotid su mamaye fiye da kima. 54%, kuma huda mai shiryarwa na duban dan tayi ba zai yiwu ba.Ana bada shawarar juyawa
4. Subclavian vein catheterization
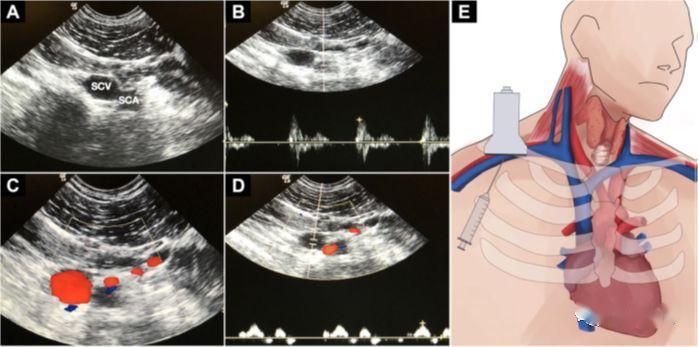
a) Ya kamata a lura cewa duban dan tayi na jijiyar subclavian yana da ɗan wahala
b) Abũbuwan amfãni: Matsayin jiki na jijiya yana da ingantacciyar abin dogaro, wanda ya dace da huda cikin jirgin sama.
c) Ƙwarewa: Ana sanya binciken tare da clavicle a cikin fossa da ke ƙasa, yana nuna hangen nesa, kuma binciken a hankali yana zamewa a tsakiya;a fasahance, jijiya axillary tana huda a nan;kunna binciken 90 digiri don nuna hangen nesa mai tsayi na jirgin jini, binciken ya dan karkata zuwa kai;bayan an daidaita binciken, ana huda allurar daga tsakiyar gefen binciken, kuma ana saka allurar a ƙarƙashin jagorar duban dan tayi na ainihin lokaci.
d) Kwanan nan, an yi amfani da ƙaramin huɗa na microconvex tare da ƙananan mitoci kaɗan don jagora, kuma binciken ya yi ƙarami kuma yana iya gani zurfi.
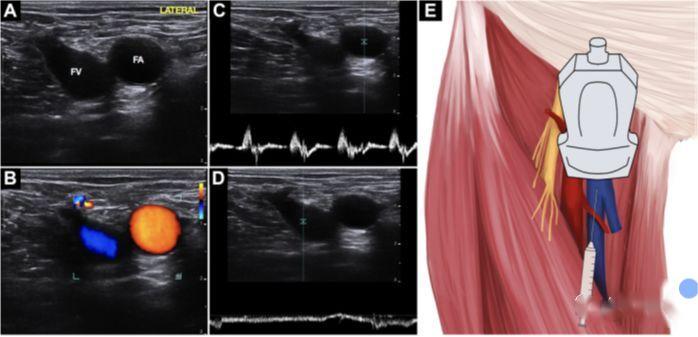
5. Catheterization na jijiyar mata
a) Abũbuwan amfãni: Ka nisantar da numfashi na numfashi da kayan aiki, babu haɗarin pneumothorax da hemothorax.
b) Babu wallafe-wallafen da yawa akan huda mai shiryarwa na duban dan tayi.Wasu mutane suna tunanin cewa abin dogara ne sosai don huda saman jiki tare da alamomin bayyane, amma duban dan tayi ba shi da inganci.Jagoran duban dan tayi ya dace sosai don FV bambancin jikin mutum da kama zuciya.
c) Matsayin kafa na kwadi yana rage haɗuwa da saman FV tare da FA, yana ɗaga kai kuma ya shimfiɗa ƙafafu a waje don faɗaɗa lumen venous.
d) Dabarar iri ɗaya ce da huda jijiyar jugular ciki
Zuciya duban dan tayi jagorar waya sakawa
1. TEE cardiac duban dan tayi yana da mafi daidaitaccen matsayi, amma yana da lahani kuma ba za a iya amfani dashi akai-akai ba.
2. Hanyar haɓakawa ta bambanta: yi amfani da microbubbles a cikin saline na al'ada mai girgiza a matsayin wakili mai banƙyama, kuma shigar da madaidaicin atrium a cikin 2 seconds bayan laminar kwarara ejection daga catheter tip
3. Yana buƙatar ƙwarewa mai yawa a cikin binciken duban dan tayi na zuciya, amma ana iya tabbatar da shi a ainihin lokacin, kyakkyawa
Duban dan tayi na huhu don kawar da pneumothorax
1. Duban dan tayi-shiryar da tsakiya venous huda ba kawai rage abin da ya faru na pneumothorax, amma kuma yana da high ji da kuma musamman ganewa na pneumothorax (mafi girma fiye da kirji X-ray).
2. Ana bada shawara don haɗa shi a cikin tsarin tabbatarwa na baya-bayan nan, wanda zai iya dubawa da sauri da kuma daidai a gefen gado.Idan an haɗa shi da sashin da ya gabata na duban dan tayi na zuciya, ana sa ran zai rage lokacin jira don amfani da catheter.
3. Lung duban dan tayi: ( ƙarin bayani na waje, don tunani kawai)
Hoton huhu na al'ada:
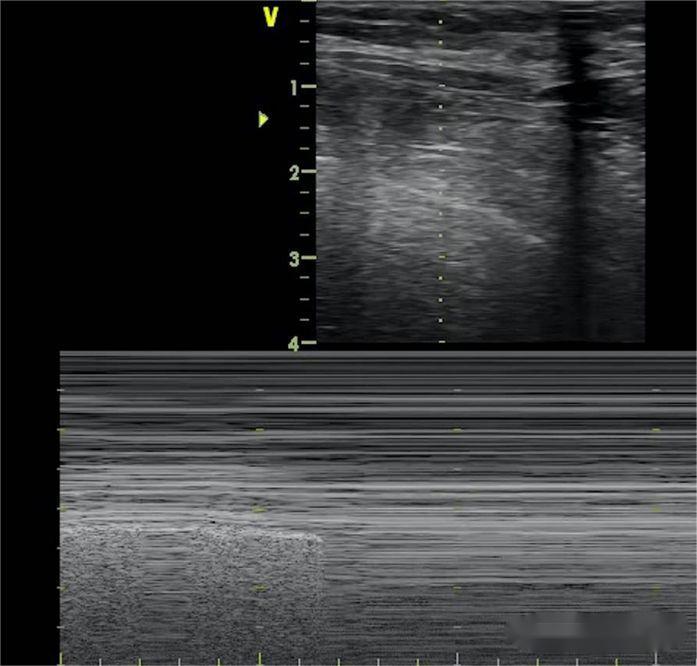
Layin A: Layin hyperechoic na pleural wanda ke zamewa tare da numfashi, yana biye da layukan da yawa daidai da shi, daidaitacce, kuma an rage shi da zurfin, wato, zamewar huhu.
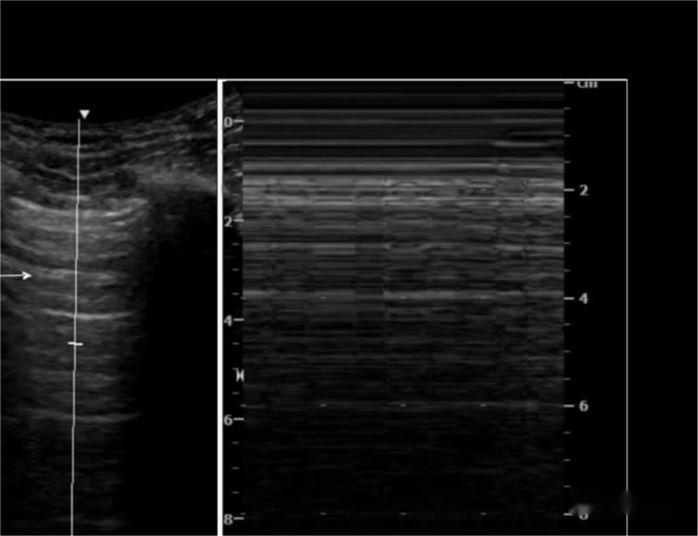
M-ultrasound ya nuna cewa layin hyperechoic da ke komawa cikin hanyar bincike tare da numfashi kamar teku ne, kuma layin pectoral mold ya kasance kamar yashi, wato, alamar bakin teku.

A wasu mutane na al'ada, sararin intercostal na ƙarshe a sama da diaphragm zai iya gano ƙasa da hotuna masu kama da laser 3 waɗanda suka samo asali daga layin pectoral mold, wanda ke shimfiɗa a tsaye a kasan allon, kuma yana amsawa tare da numfashi - layin B.
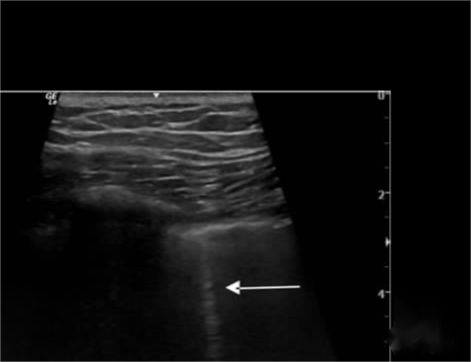
Hoton Pneumothorax:
Layin B ya ɓace, zamewar huhu ya ɓace, kuma alamar rairayin bakin teku ta maye gurbin ta da alamar barcode.Bugu da ƙari, ana amfani da alamar alamar huhu don sanin girman pneumothorax, kuma wurin huhu ya bayyana inda alamar bakin teku da alamar lambar wucewa ta bayyana.
Horon CVC da Ultrasound ke Jagoranta
1. Rashin daidaituwa akan matakan horo da takaddun shaida
2. Tunanin cewa dabarun shigar makanta sun ɓace a cikin koyon fasahar duban dan tayi;duk da haka, yayin da fasahar duban dan tayi ya zama mafi tartsatsi, zabi tsakanin aminci na haƙuri da kiyaye hanyoyin da za a iya amfani da su ba za a yi la'akari da su ba.
3. Ya kamata a yi la'akari da ƙwarewar asibiti ta hanyar lura da aikin asibiti maimakon dogaro da adadin hanyoyin.
a karshe
Makullin ingantacciyar hanya da aminci ga CVC mai jagorar duban dan tayi shine sani game da ramummuka da iyakokin wannan fasaha ban da horon da ya dace.
Lokacin aikawa: Nuwamba-26-2022