Basic components of an anesthesia machine
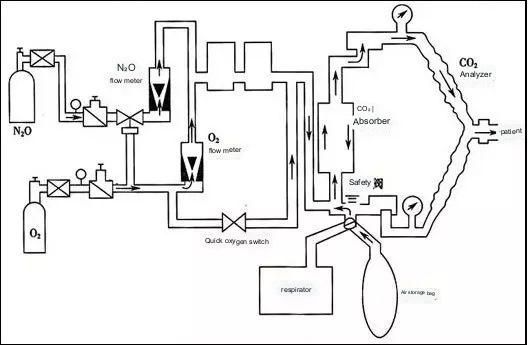
During the operation of the anesthesia machine, the high-pressure gas (air, oxygen O2, nitrous oxide, etc.) is decompressed through the pressure reducing valve to obtain a low-pressure and stable gas, and then the flow meter and the O2-N2O ratio control device are adjusted to generate a certain flow rate. And the proportion of mixed gas, into the breathing circuit.
The anesthesia medicine generates anesthetic vapor through the volatilization tank, and the required quantitative anesthetic vapor enters the breathing circuit and is sent to the patient together with the mixed gas.
It mainly consists of gas supply device, evaporator, breathing circuit, carbon dioxide absorption device, anesthesia ventilator, anesthesia waste gas removal system, etc.
- Air supply device
This part is mainly composed of air source, pressure gauge and pressure reducing valve, flow meter and proportioning system.
The operating room is generally provided with oxygen, nitrous oxide, and air by a central air supply system. The gastrointestinal endoscopy room is generally a cylinder gas source. These gases are initially under high pressure and must be decompressed in two steps before they can be used. So there are pressure gauges and pressure relief valves. The pressure reducing valve is to reduce the original high-pressure compressed gas to a safe, constant low-pressure gas for the safe use of anesthesia machines. Generally, when the high-pressure gas cylinder is full, the pressure is 140kg/cm². After passing through the pressure reducing valve, it will finally drop to about 3~4kg/cm², which is 0.3~0.4MPa that we often see in textbooks. It is suitable for constant low pressure in anesthesia machines.
The flow meter accurately controls and quantifies the gas flow to the fresh gas outlet. The most common one is the suspension rotameter.
After the flow control valve is opened, the gas can freely pass through the annular gap between the float and the flow tube. When the flow rate is set, the buoy will balance and rotate freely at the set value position. At this time, the upward force of the air flow on the buoy is equal to the gravity of the buoy itself. When in use, do not use too much force or overtighten the rotary knob, otherwise it will easily cause the thimble to bend, or the valve seat will deform, causing the gas to fail to close completely and cause air leakage.
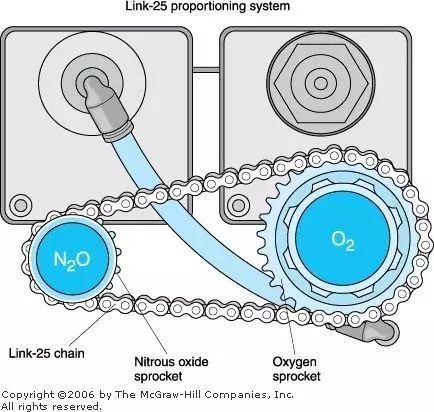
In order to prevent the anesthesia machine from outputting hypoxic gas, the anesthesia machine also has a flow meter linkage device and an oxygen ratio monitoring device to keep the minimum oxygen concentration output by the fresh gas outlet at about 25%. The principle of gear linkage is adopted. On the N₂O flowmeter button, the two gears are connected by a chain, O₂ rotates once, and N₂O rotates twice. When the needle valve of the O₂ flowmeter is unscrewed alone, the N₂O flowmeter remains still; when the N₂O flowmeter is unscrewed, the O₂ flowmeter is linked accordingly; when both flowmeters are opened, the O₂ flowmeter is gradually closed, and the N₂O flowmeter It also decreased in conjunction with it.
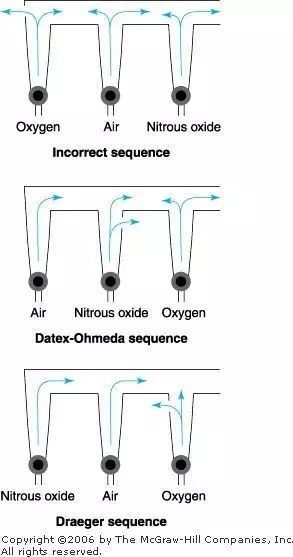
Install the oxygen flow meter closest to the common outlet. In case of a leak at the oxygen upwind position, most of the loss is N2O or air, and the loss of O2 is the least. Of course, its sequence does not guarantee that hypoxia due to flow meter rupture will not occur.
2.Evaporator
An evaporator is a device that can convert a liquid volatile anesthetic into a vapor and input it into the anesthesia circuit in a certain amount. There are many types of evaporators and their characteristics, but the overall design principle is shown in the figure.
The mixed gas (that is, O₂, N₂O, air) enters the evaporator and is divided into two paths. One path is a small airflow not exceeding 20% of the total amount, which enters the evaporation chamber to bring out the anesthetic vapor; 80% of the larger gas flow directly enters the main airway and enters the anesthesia loop system. Finally, the two airflows are combined into a mixed airflow for the patient to inhale, and the distribution ratio of the two airflows depends on the resistance in each airway, which is regulated by the concentration control knob.
3.Breathing circuit
Now the most commonly used clinically is the circulatory loop system, that is, the CO2 absorption system. It can be divided into semi-closed type and closed type. The semi-closed type means that part of the exhaled air is reinhaled after being absorbed by the CO2 absorbent; the closed type means that all the exhaled air is reinhaled after being absorbed by the CO2 absorbent. Looking at the structure diagram, the APL valve is closed as a closed system, and the APL valve is opened as a semi-closed system. The two systems are actually the two states of the APL valve.
It mainly consists of 7 parts: ① fresh air source; ② inhalation and exhalation one-way valve; ③ threaded pipe; ④ Y-shaped joint; ⑤ overflow valve or pressure reducing valve (APL valve); ⑥ air storage bag; The inspiratory and exhalation one-way valve can ensure the one-way flow of gas in the threaded tube. In addition, the smoothness of each component is also particular. One is for the one-way flow of gas, and the other is to prevent repeated inhalation of exhaled CO2 in the circuit. Compared with the open breathing circuit, this kind of semi-closed or closed breathing circuit can allow rebreathing of breathing gas, reduce the loss of water and heat in the respiratory tract, and also reduce the pollution of the operating room, and the concentration of anesthetics is relatively stable. But there is an obvious disadvantage, it will increase the breathing resistance, and the exhaled air is easy to condense on the one-way valve, which requires timely cleaning of the water on the one-way valve.
Here I would like to clarify the role of the APL valve. There are a few questions about it that I can’t figure out. I asked my classmates, but I couldn’t explain clearly; I asked my teacher before, and he also showed me the video, and it was clear at a glance. APL valve, also called overflow valve or decompression valve, the English full name is adjustable pressure limiting, no matter from Chinese or English, everyone must have a little understanding of the way, this is a valve that limits the pressure of the breathing circuit. Under manual control, if the pressure in the breathing circuit is higher than the APL limit value, the gas will run out from the valve to reduce the pressure in the breathing circuit. Think about it when assisted ventilation, sometimes pinching the ball is more inflated, so I quickly adjust the APL value, the purpose is to deflate and reduce pressure. Of course, this APL value is generally 30cmH2O. This is because generally speaking, the peak airway pressure should be <40cmH2O, and the average airway pressure should be <30cmH2O, so the possibility of pneumothorax is relatively small. The APL valve in the department is controlled by a spring and marked with 0~70cmH2O. Under machine control, there is no such thing as an APL valve. Because the gas no longer passes through the APL valve, it is connected to the ventilator. When the pressure in the system is too high, it will release the pressure from the excess gas discharge valve of the bellows of the anesthesia ventilator to ensure that the circulatory system will not cause barotrauma to the patient. But for the sake of safety, the APL valve should be set to 0 habitually under machine control, so that at the end of the operation, the machine control will be switched to manual control, and you can check whether the patient is breathing spontaneously. If you forget to adjust the APL valve, the gas will only It can enter the lungs, and the ball will become more and more bulging, and it needs to be deflated immediately. Of course, if you need to inflate the lungs at this time, adjust the APL valve to 30cmH2O
4. Carbon dioxide absorption device
Absorbents include soda lime, calcium lime, and barium lime, which are rare. Because of the different indicators, after absorbing CO2, the color change is also different. The soda lime used in the department is granular, and its indicator is phenolphthalein, which is colorless when fresh and turns pink when exhausted. Do not ignore it when checking the anesthesia machine in the morning. It is best to replace it before the operation. I made this mistake.
Compared with the ventilator in the recovery room, the breathing pattern of the anesthesia ventilator is relatively simple. The required ventilator can only change the ventilation volume, respiratory rate and respiratory ratio, can run IPPV, and can basically be used. In the inspiratory phase of the human body’s spontaneous breathing, the diaphragm contracts, the chest expands, and the negative pressure in the chest increases, causing a pressure difference between the airway opening and the alveoli, and gas enters the alveoli. During mechanical respiration, positive pressure is often used to form a pressure difference to push the anesthesia air into the alveoli. When the positive pressure is stopped, the chest and lung tissue elastically retracts to generate a pressure difference from the atmospheric pressure, and the alveolar gas is discharged out of the body. Therefore, the ventilator has four basic functions, namely inflation, conversion from inhalation to exhalation, discharge of alveolar gas, and conversion from exhalation to inhalation, and the cycle repeats in turn.
As shown in the figure above, the driving gas and the breathing circuit are isolated from each other, the driving gas is in the bellows box, and the breathing circuit gas is in the breathing bag. When inhaling, the driving gas enters the bellows box, the pressure inside it rises, and the release valve of the ventilator is closed first, so that the gas will not enter the residual gas removal system. In this way, the anesthetic gas in the breathing bag is compressed and is released into the patient’s airway. When exhaling, the driving gas leaves the bellows box, and the pressure in the bellows box drops to atmospheric pressure, but the exhalation first fills the exhalation bladder. This is because there is a small ball in the valve, which has weight. Only when the pressure in the bellows exceeds 2 ~3cmH₂O, this valve will open, that is, excess gas can pass through it into the residual gas removal system. To put it bluntly, this ascending bellows will produce PEEP (positive end-expiratory pressure) of 2~3cmH2O. There are 3 basic modes for the breathing cycle switching of the ventilator, namely constant volume, constant pressure and timing switching. At present, most anesthesia respirators use the constant volume switching mode, that is, during the inspiratory phase, the preset tidal volume is sent into the patient’s respiratory tract until the alveoli to complete the inspiratory phase, and then switch to the preset expiratory phase , thereby forming a breathing cycle, wherein the preset tidal volume, breathing rate and breathing ratio are three main parameters for adjusting the breathing cycle.
6.Exhaust gas removal system
As the name suggests, it is to deal with exhaust gas and prevent pollution in the operating room. I don’t care much about this at work, but the exhaust pipe must not be blocked, otherwise the gas will be squeezed into the patient’s lungs, and the consequences can be imagined.
To write this is to have a macroscopic understanding of the anesthesia machine. Connecting these parts and moving them is the working state of the anesthesia machine. Of course, there are still many details that need to be considered slowly, and the ability is limited, so I will not get to the bottom of it for the time being. Theory belongs to theory. No matter how much you read and write, you still have to put it into work, or practice. After all, it is better to do well than to say well.
Post time: Jun-05-2023