Global status of chronic kidney disease
Epidemiological surveys have shown that chronic kidney disease has become one of the major diseases threatening public health worldwide. In recent years, statistics show that in developed countries (such as the United States and the Netherlands), about 6.5% to 10% of the general population has different degrees of kidney disease, of which the number of kidney disease in the United States has exceeded 20 million, and hospitals treat kidney disease patients up to more than 1 million each year. The total number of patients with end-stage renal disease in China is also increasing, and it is expected that the number of patients with end-stage renal disease in China will exceed 4 million by 2030.
Hemodialysis (HD) is one of the renal replacement therapy for patients with acute and chronic renal failure.
The establishment of an effective vascular access is the prerequisite for the smooth progress of hemodialysis. The quality of vascular access directly affects the quality of dialysis and life of patients. Proper use and careful protection of vascular access can not only prolong the service life of vascular access, but also prolong the life of dialysis patients, so vascular access is called the “lifeline” of dialysis patients.
Clinical application of ultrasound in AVF
Experts of vascular access group believe that AVF should be the first choice for vascular access. Due to the non-renewable, limited number of vascular resources, and can not be completely replaced, in order to maximize the service life of the patient access, standardized use and maintenance of arteriovenous fistula, and effectively avoid puncture related complications are the problems that have attracted the attention of clinicians and nurses.
To establish the preoperative vascular evaluation of arteriovenous fistula (AVF)
1) Whether the blood vessels are normal: tortuosity, stenosis and dilatation
2) whether the vessel wall is smooth, whether there is plaque echo, whether there is fracture or defect, and whether there is dissection
3) whether there are thrombi and other echoes in the lumen
4) Whether the color blood flow filling is complete and whether the direction and speed of blood flow are abnormal
5) Blood flow assessment
The picture shows Professor Gao Min treating the patient at the bedside
Monitoring of internal fistulas
Since the establishment of internal fistula for patients is the first step of “the long march”, AVF before using ultrasonic measurement vascular diameter and blood flow naturally, when assessing the fistula can, have mature standards, to measure whether the patients with fistula in the data using standard, ultrasound is undoubtedly the most intuitive and accurate method.
AVF monitoring: Ultrasound monitoring was performed once a month
1) Blood flow
2) Vessel diameter
3) Whether the anastomosis is narrow and whether there is thrombosis (if there is thrombosis, it is necessary to increase the balloon)
Mature judgment of autogenous arteriovenous fistula
Regardless of the recommended time to start puncture, the prerequisite must be after the internal fistula has matured.
It is generally believed that the maturity of internal fistula should meet the three “6″ criteria:
1) arteriovenous fistula flow > 600ml/min (2019 Chinese expert consensus on vascular access for hemodialysis: > 500 ml/min)
2) diameter of puncture vein > 6mm (2019 Chinese expert consensus on vascular access for hemodialysis: > 5 mm)
3) Venous subcutaneous depth & LT; 6mm, and there should be enough blood vessel puncture distance to meet the use of hemodialysis.
In most cases, arteriovenous fistulas with palpable veins and good tremor can be successfully punctures within 4 weeks of their establishment.
Assessment and maintenance
It is very important to regularly evaluate and monitor the clinical indicators of arteriovenous fistula and hemodialysis adequacy after operation.
Good assessment and monitoring methods include
① Access blood flow monitoring: it is recommended to monitor once a month;
② Physical examination: it is recommended that every dialysis should be checked, including inspection, palpation and auscultation;
③ Doppler ultrasound: recommended once every 3 months;
④ Non-urea dilution method is recommended to measure recycling once every 3 months;
⑤ Direct or indirect static venous pressure detection is recommended once every 3 months.
When autologous AVF cannot be established, the secondary choice should be graft internal fistula (AVG). Whether it is to establish AVF or AVG, ultrasound is essential for preoperative evaluation of blood vessels, intraoperative guidance of puncture, postoperative evaluation and maintenance.
PTA was performed under ultrasound guidance
The inevitable complication of arteriovenous fistula is stenosis. Long-term high-speed blood flow can cause reactive hyperplasia of venous intima of internal fistula, leading to vascular stenosis and insufficient blood flow, affecting the effect of dialysis, and leading to fistula occlusion, thrombosis and failure when the stenosis is severe.
At present the mainstream operation for treatment of internal fistula stenosis for ultrasound guided arteriovenous fistula stenosis in keratoplasty (PTA), balloon expansion treatment by skin biopsy in patients with fistula in blood vessels, into the catheter balloon expansion, in under the guidance of ultrasound for vascular stenosis site expansion, rectify narrow parts, restore normal blood vessel diameter, so as to prolong the service life of the patients with arteriovenous internal fistula.
PTA under the guided by ultrasound, is convenient, no radiation damage, no contrast agent damage, it can display and vascular occlusion lesions around the situation, the measured blood flow parameters and evaluate blood flow, and can be immediately after the success as a vascular access for hemodialysis, don’t need a temporary catheter, with a safe, effective and the characteristics of small trauma, rapid recovery, reduce the patient’s pain, The processing process is simplified.
Clinical application of ultrasound in central venous catheterization
Before establishing a central venous catheter, ultrasound should be used to assess the condition of the internal jugular vein or femoral vein, especially in patients with a history of previous intubation, and ultrasound should be used to check for vein stenosis or occlusion. Under the guidance of ultrasound, ultrasound, as the doctor’s “third eye”, can see more clearly and truly.
1) Evaluate the diameter, depth and patency of the puncture vein
2) The puncture needle into the blood vessel could be visualized
3) Real-time display of the trajectory of the needle in the blood vessel to avoid intimal injury
4) Avoid the occurrence of complications (accidental artery puncture, hematoma formation or pneumothorax)
5) To improve the success rate of the first puncture
Clinical application of ultrasound in peritoneal dialysis catheterization
Peritoneal dialysis is a kind of renal replacement therapy, which mainly uses the condition of own peritoneum to carry out renal replacement therapy. Compared with hemodialysis, it has the characteristics of simple operation, self-dialysis and maximum protection of residual renal function.
The choice of the placement of peritoneal dialysis catheter on the body surface is a very important step in the establishment of unobstructed peritoneal dialysis access. In order to maintain the patency of peritoneal dialysis drainage and reduce the occurrence of catheterization complications, it is necessary to be familiar with the anatomical structure of the anterior abdominal wall and choose the most appropriate insertion point of the peritoneal dialysis catheter.
Percutaneous placement of peritoneal dialysis catheter under ultrasound guidance is minimally invasive, economical, easy to operate, more safe, intuitive and reliable.
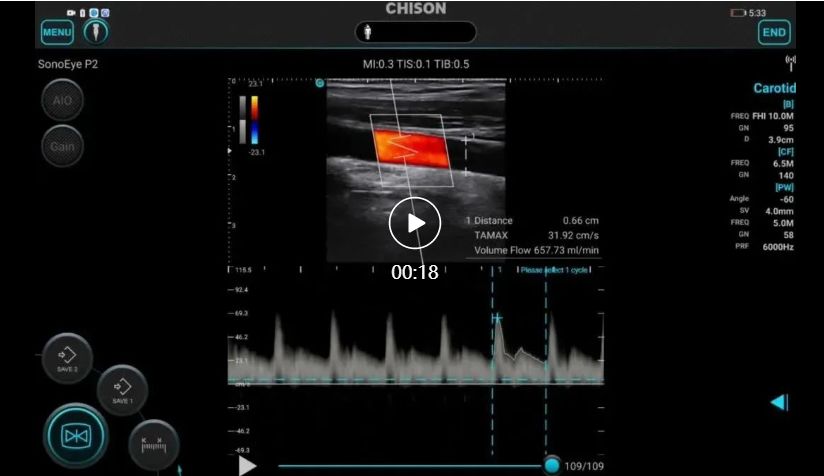
SonoEye palmar ultrasonication was used for vascular access
SonoEye is ultra-portable and small, does not occupy the bedside area, is easy to check, can be directly connected to the phone or tablet, open the application at any time.
The picture shows Professor Gao Min treating the patient at the bedside
Chison palm ultrasound has diagnostic images and is equipped with an intelligent blood flow measurement package, which automatically envelopes and gives bleeding flow results.
Ultrasound-guided puncture of internal fistula can greatly improve the success rate of puncture and reduce the incidence of complications such as hematoma and pseudoaneurysm.
Welcome to contact us for more professional medical products and knowledge.
Contact Details
Icy Yi
Amain Technology Co., Ltd.
Mob/WhatsApp: 008617360198769
E-mail: amain006@amaintech.com
Linkedin: 008617360198769
Tel.: 00862863918480
Post time: Nov-03-2022